 History
HistoryOn Saturday April 29, 2006 at about 7:20 PM my wife and I were boarding an airplane to return home from a trip to a distant city. Our four-year-old daughter and younger son had spent the day with my parents and sister and were enjoying the evening with them at a local park. Our daughter was riding on a swing when she suddenly let go and fell to the ground, landing upside-down directly on her head with her neck flexed. She did not lose consciousness and appeared to be fine at the scene of the accident, although she was crying from the obvious pain of her fall.
As my father carried her the short distance to his house, she told him through her tears: "Grandpa, please just say a prayer for me so that I'll be able to stop crying." It was a plea of perfect faith that she would repeat several other times to caregivers who assisted her before my wife and I arrived on the scene.
Upon arriving home several minutes later with her, our relatives noticed that she exhibited weakness in the left side of her body and immediately called 911. The paramedics arrived soon thereafter and rushed her to the top trauma hospital in our area, where she received excellent and timely care.
In the meantime, my wife and I arrived at the airport and checked our voicemail. While we were in flight I had received a message from my father indicating that an accident had occurred and we should meet him at the hospital as soon as possible. We sprinted through the terminal to the garage and quickly drove to the hospital.
I'll never forget the sight of our daughter lying on a bed in the trauma room among victims of various other accidents on a busy Saturday night. Her left arm and leg were motionless, as was the left side of her face. When she saw us she struggled to speak through her half-motionless lips and tongue and sobbed: "I fell out of a swing!" I felt profoundly helpless. I couldn't hold her or even reassure her that everything would be alright.
The trauma team worked quickly and efficiently. By the time we had arrived, our daughter had already undergone a CT scan that identified a right occipital skull fracture and ruled out any damage to her spine. She soon underwent a CT with contrast that ruled out any hemorrhage in her brain. At that point it was determined that she would likely not need emergency surgery that night, and she was transferred to the pediatric intensive care unit (PICU) for observation until the following morning when she would be able to undergo an MRI scan of her head.
My wife and I agreed that she would spend the night in the PICU with our daughter while I went home to catch a few hours of sleep (it was now after 2:00 AM). I would return in the morning so she could do the same. We were hopeful that her apparent neurological problems were a temporary result of a concussion incident to the skull fracture. I brought her clothes and car seat with me when I returned to the hospital the following morning in anticipation of her imminent discharge.
The next day while my wife slept at home, our daughter underwent an MRI study. She was sedated to prevent her from moving and thereby interfering with the exam. We were blessed to be prioritized at the top of the list of 17 MRIs that were ordered overnight in this busy hospital. After an ad-hoc team consisting of the MRI technician, the anesthesiologist, the PICU nurse, the PICU resident, another random nurse, and ultimately the attending PICU intensivist spent 40 minutes figuring out how to use the two-day-old MRI anesthesia IV infusion pump, the rest of the procedure went fairly quickly.
By mid-afternoon, once the attending neurologist and radiologist had reviewed the results of the MRI, the neurologist came to the PICU to deliver the news that our daughter "appears to have suffered a disruption in the circulation of blood within her brain." "You mean she's had a stroke?" I asked. "Precisely," he said. I was stunned beyond words by the gravity of the situation. The night before, after encouraging results of her CT scans, I had imagined that our daughter had a concussion and simple skull fracture and would be able to return home soon. Now in an instant I understood that she had permanent brain damage that would require months of therapy to address, and that her outcome was far from certain.
The neurologist continued by explaining that while our daughter may recover some of her motor function, it was likely that she may never recover the level of function that she enjoyed before she suffered her stroke. He offered genuine sympathy for her condition and explained that a stroke resulting from a bump on the head seemed to be extremely rare. While he wasn't a pediatric specialist, he had briefly searched the published literature and found only one case -- that of a Turkish boy who fell off a fence and landed on his head -- that seemed to match that of our daughter. He said that he wondered whether the fall caused the stroke or vice-versa.
Since our daughter's stroke was ischemic in nature -- caused by a lack of blood flow rather than a hemorrhage -- the neurologist indicated that he would order an array of lab tests to help understand if some underlying blood or vascular disorder had led to this episode. After explaining all of this to me, he left the PICU and I was left to ponder what it meant.
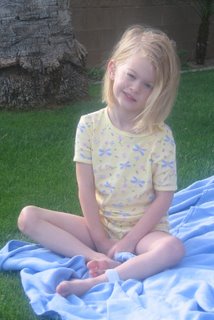
 Our daughter was sleeping peacefully as I sat and considered what the news I had just received might mean to her and to our family. I had managed to keep my composure as the neurologist delivered the bad news, but a minute or two after he left the room I completely broke down. I struggled to imagine how this beautiful, active, talented little girl could have her life disrupted in an instant by such a random event. I wondered how she would cope with the possibility that she may never be able to ride her bike, play soccer, run, or play the piano again. I wondered how she would feel knowing that she might not be able to learn to play baseball or the violin as she had planned. I wondered how her friends would treat her, whether other children would tease her, whether she would be socially accepted, whether she would have the opportunity to marry. I wondered whether a possible underlying condition might prevent her from having children of her own. I dreaded the thought that she might be predisposed to suffering another stroke that would cause further impairment, or worse, end her young life. The anxiety I had felt about her present condition soon evaporated and was replaced by profound sorrow over what the future might hold.
Our daughter was sleeping peacefully as I sat and considered what the news I had just received might mean to her and to our family. I had managed to keep my composure as the neurologist delivered the bad news, but a minute or two after he left the room I completely broke down. I struggled to imagine how this beautiful, active, talented little girl could have her life disrupted in an instant by such a random event. I wondered how she would cope with the possibility that she may never be able to ride her bike, play soccer, run, or play the piano again. I wondered how she would feel knowing that she might not be able to learn to play baseball or the violin as she had planned. I wondered how her friends would treat her, whether other children would tease her, whether she would be socially accepted, whether she would have the opportunity to marry. I wondered whether a possible underlying condition might prevent her from having children of her own. I dreaded the thought that she might be predisposed to suffering another stroke that would cause further impairment, or worse, end her young life. The anxiety I had felt about her present condition soon evaporated and was replaced by profound sorrow over what the future might hold.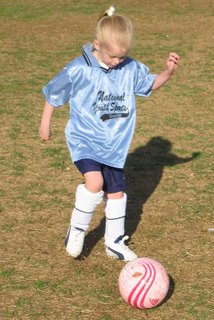 I called my wife to deliver the news I had heard from the neurologist and broke down again when I heard her own sadness. We communicated the news to our extended family members. Many of them came to visit as the afternoon turned into our second night in the PICU.
I called my wife to deliver the news I had heard from the neurologist and broke down again when I heard her own sadness. We communicated the news to our extended family members. Many of them came to visit as the afternoon turned into our second night in the PICU.When I awoke on Monday morning, my wife called to inform me that our daughter had been judged sufficiently stable to move to a PICU step-down bed and would soon be transferred to the general pediatric ward where she could be free of her IV and monitors. After the MRI was done on Sunday morning, we had been anxious to have our daughter's cervical collar removed from her neck so that she could be a bit more comfortable in her bed. We were frustrated by the fact that the intensivists deferred to the trauma physicians, who in turn deferred to the neurologist, who deferred back to the trauma physicians on this decision. On Monday morning the neurologist did a quick physical exam of our daughter's neck and ordered the collar removed. She was transferred to the pediatric ward soon thereafter, into a room she would share with three other girls between the ages of 8 and 17.
 Prior to the collar being removed, an echocardiogram was performed on orders from the neurologist to attempt to rule out any heart abnormalities that could have generated an embolism that may have caused the stroke. Because we did not hear any news regarding the echocardiogram on Monday we assumed all was well, that is until the test was repeated early Tuesday morning because the first test was inconclusive. A visit by the trauma physician (our daughter was still registered under the trauma service) later that morning struck fear into my heart: The initial echocardiogram showed what appeared to be a "mass" in the right atrium. In addition, further review of her initial radiology results showed two calcified areas in her brain, likely the result of previous strokes. Our anxiety about the future was amplified by the speculation that a heart condition likely existed and that she had already suffered two additional strokes without our knowledge. We began to fear that her stroke would recur in the future.
Prior to the collar being removed, an echocardiogram was performed on orders from the neurologist to attempt to rule out any heart abnormalities that could have generated an embolism that may have caused the stroke. Because we did not hear any news regarding the echocardiogram on Monday we assumed all was well, that is until the test was repeated early Tuesday morning because the first test was inconclusive. A visit by the trauma physician (our daughter was still registered under the trauma service) later that morning struck fear into my heart: The initial echocardiogram showed what appeared to be a "mass" in the right atrium. In addition, further review of her initial radiology results showed two calcified areas in her brain, likely the result of previous strokes. Our anxiety about the future was amplified by the speculation that a heart condition likely existed and that she had already suffered two additional strokes without our knowledge. We began to fear that her stroke would recur in the future.
By Tuesday evening, results from the second echocardiogram were in and showed no heart abnormalities. What a relief! The first echocardiogram could not visualize the right atrium completely because the cervical collar was in the way. I pondered the cost of poor communication and lack of clear decision ownership among the three physicians: A repeated test, repeated interpretation of the test by a pediatric cardiologist and his peers, and a gut-wrenching day for the family of a sick little girl.

As Wednesday dawned we hoped that we would soon be transferred to the Children's Hospital, an environment much more conducive to healing than is the trauma hospital that is designed to save lives. We had spent the past day trying to do anything possible to avoid the room that our daughter shared with the three older girls, whose many relatives didn't seem to realize the correlation between peace, quiet, and rest. We took our daughter's meals outside and had picnics in the "healing garden", where she enjoyed seeing the little sparrows and other birds eat the crumbs she would flick at them. We even saw a hummingbird take a bath in a fountain inside the garden, which she thought was pretty fun. By this time she had regained enough strength and motor control in her trunk that she was able to sit on her own for short periods of time.
 Wednesday ground on, and our frustration with our situation mounted. The hospital staff had determined to do little else besides monitor our daughter's vital signs and manage her pain until she could be transferred to the children's hospital for rehab and to consult with hematology about the possible cause of her stroke. But there were no beds available in the children's hospital rehab unit. We were stuck until someone was discharged and a bed was available. In the meantime, we were transferred to a more-private room that would afford our daughter more quiet rest overnight. We were assured that we were at the top of the list to be transferred to rehab at the children's hospital, and that a bed should be available on Thursday morning.
Wednesday ground on, and our frustration with our situation mounted. The hospital staff had determined to do little else besides monitor our daughter's vital signs and manage her pain until she could be transferred to the children's hospital for rehab and to consult with hematology about the possible cause of her stroke. But there were no beds available in the children's hospital rehab unit. We were stuck until someone was discharged and a bed was available. In the meantime, we were transferred to a more-private room that would afford our daughter more quiet rest overnight. We were assured that we were at the top of the list to be transferred to rehab at the children's hospital, and that a bed should be available on Thursday morning.
<< Home